Medicare patients cheered when the Inflation Reduction Act capped monthly insulin costs at $35. Then drug manufacturers controlling 90% of the market set this $35 cap for everyone by bypassing the PBM middlemen. To protect their black box of profits, insiders expect PBMs to raise employer premiums.
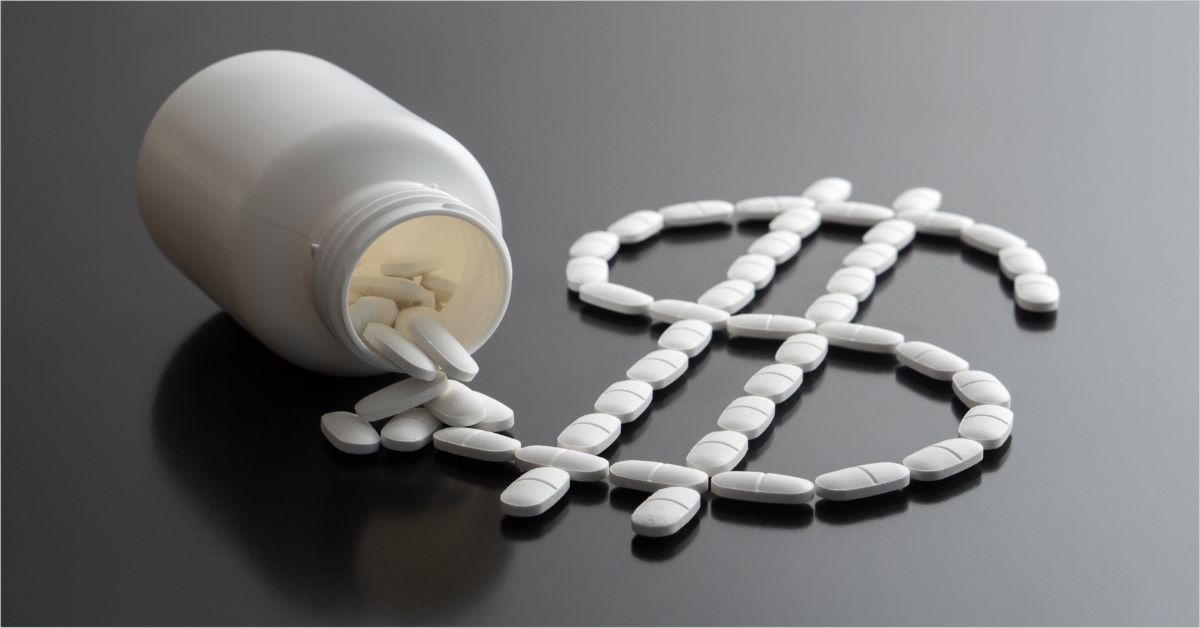
Consider how much money is at stake. Patients who paid over $1,000 per month for insulin in 2018 are now paying only $35 in 2023. And despite slashing insulin costs by 70%, pharmaceutical companies will still profit handsomely. It’s a win-win for all stakeholders except the PBMs.
This huge gap represents the “60% or 70% of fees” taken by PBMs, who act as intermediaries between drug manufacturers and pharmacies in the supply chain. These fees are a driving force behind the rise in prescription drug costs. Such predatory business practices are all about profits, so a loss here must be offset by a gain somewhere else. Next target, employers.
Employers can fight back and save money by axing their PBM and working with a modern health plan that delivers an ethically-grounded pharmacy program and formulary based on science and clinical value with advanced cost-plus pricing technology for net lowest cost results. Transparent pharmacy services administration ensures that what’s paid at the pharmacy is what the employer plan sponsor pays and 100% of rebates paid monthly.
It’s time to eliminate the dubious fees and questionable practices that raise costs for employers and their members.