A report by the PBM Accountability Project reveals the details of PBMs’ “evolving business models and revenue.” Despite the available financial data, the authors could not identify “the source of nearly 40% of PBMs’ total gross profit.” Can this “business as usual” become a catalyst for change?
The coalition of pharmacy, labor, healthcare, business, and patient advocacy groups that supports the PBM Accountability Project certainly hopes so.
A Sea of Shifting Profits
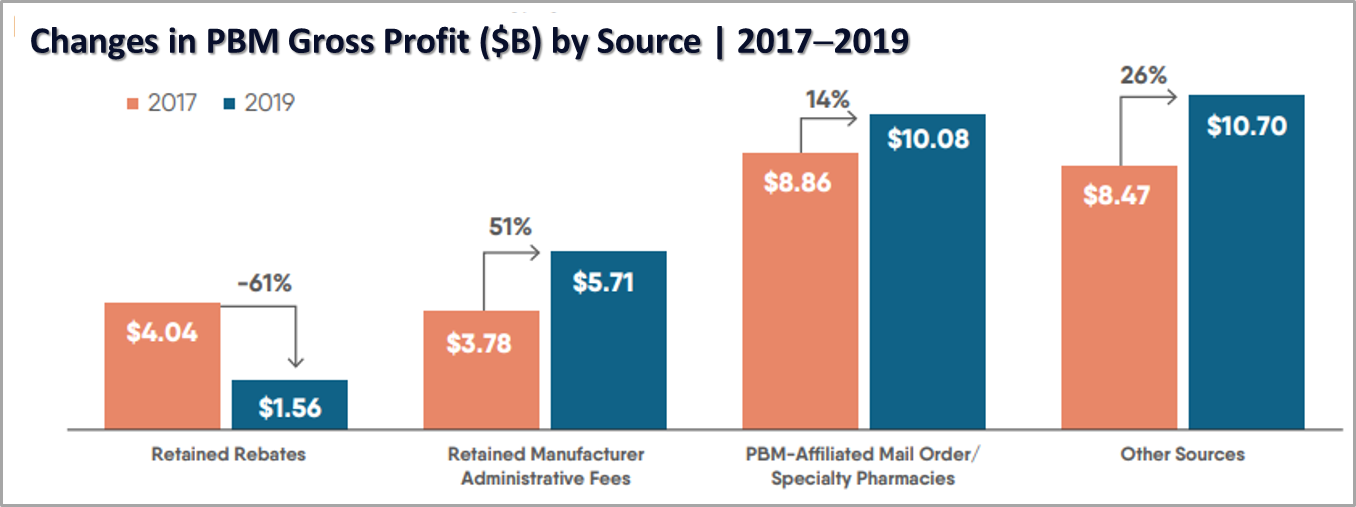
As described in the report, revenue flows to PBMs from multiple stakeholders in the supply chain, not just payer clients. And gross profit is generated through multiple sources and business activities, including but not limited to retained rebates, retained manufacturer administrative service fees, and their own mail order/specialty pharmacies.
So where is that 40% of unaccounted-for profit hiding? Potential sources may include “spread pricing, pharmacy fees and clawbacks, fees collected from payers, and other non-administrative fees collected from manufacturers.”
Despite stakeholders demanding more transparency, PBMs play shell games by rebalancing revenue streams and identifying new ones to offset those with smaller profits. Their results have been quite successful: a 12% increase in overall gross profit, from $25 billion in 2017 to $28 billion in 2019.
 Source: PBM Accountability Project: Understanding the Evolving Business Models and Revenue of Pharmacy Benefit Managers 2021
Source: PBM Accountability Project: Understanding the Evolving Business Models and Revenue of Pharmacy Benefit Managers 2021
PBMs: A Black Box of Control
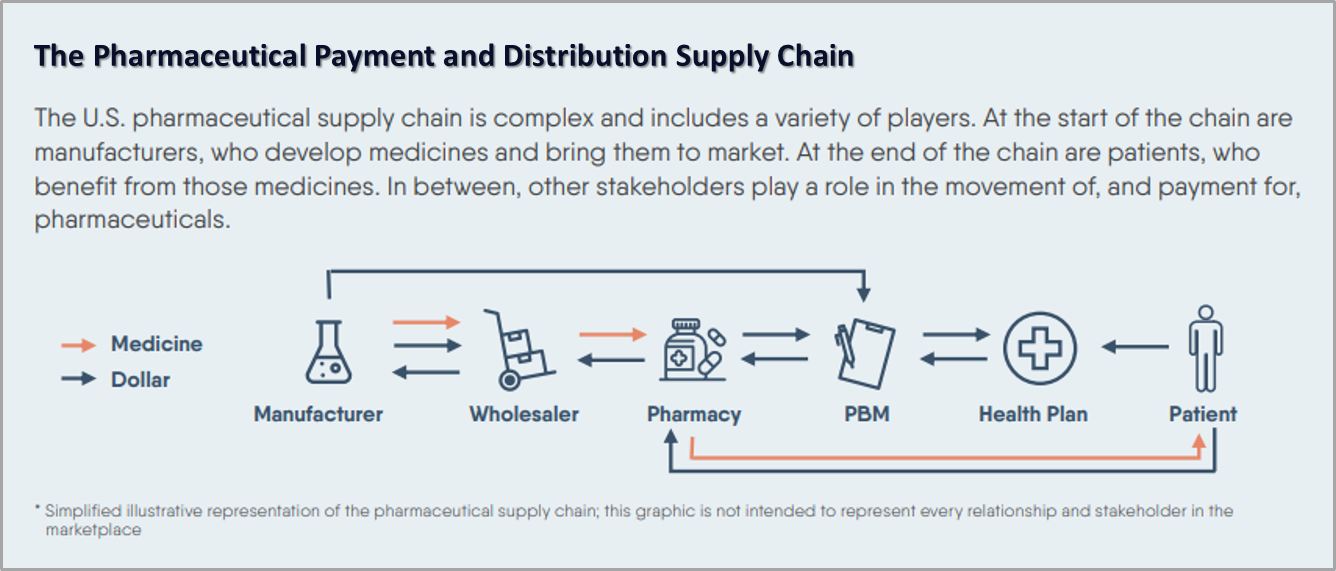
Efforts to ensure that public and private sector health plans don’t overpay for prescription medicines often focus on government control of drug prices through legislation, including through the Build Back Better Act currently under debate. Given the complexity of the pharmaceutical supply chain, which is the most effective point to apply such legislation?
 Source: PBM Accountability Project: Understanding the Evolving Business Models and Revenue of Pharmacy Benefit Managers 2021
Source: PBM Accountability Project: Understanding the Evolving Business Models and Revenue of Pharmacy Benefit Managers 2021
In an interview by AIS Health, Lindsay Bealor Greenleaf, vice president at ADVI Health, acknowledges that “the legislation does impose some new transparency requirements on PBMs,” but that it is setting “government price controls on manufacturers while letting the PBMs completely off the hook.”
Greenleaf asserts that PBMs “operate in a black box, and they profit most from drugs with the highest list prices, and then they make patients pay coinsurance based off those inflated list prices.” Holding so much power is a dangerous combination that must be addressed to hold PBMs accountable for their role in rising prescription drug costs.
If PBMs don’t innovate and proactively adopt reforms and the government doesn’t force the issue, “the biggest hope for change” is likely to come from employers and other clients of PBMs, Greenleaf says. “The hope is that they keep stepping up and saying, ‘What’s going on here, am I getting the best deal, and even if I am getting a good deal, how good of a deal are you getting?’”
Employers can seek out ethical, member-focused prescription drug plans like VitoriRx to eliminate the predatory practices and half-measures of transparency from legacy PBMs. They can also support groups like the PBM Accountability Project, whose sponsors demand lower drug prices and cost increases and greater accountability and transparency from PBMs.




