JAMA | Broken Health Benefits Market Reduces Quality of Life
A recent article posted to JAMA Network reveals how the dysfunctional interests of insurers, hospitals, pharmaceutical companies, and PBMs ultimately reduce quality of life for U.S. employees through financial distress induced by the health benefits market.
According to the authors, “It is assumed that insurers compete intensely to improve the value received by employers and employees by negotiating to keep prices down and advocating for employers and employees.” This is not the case, however.
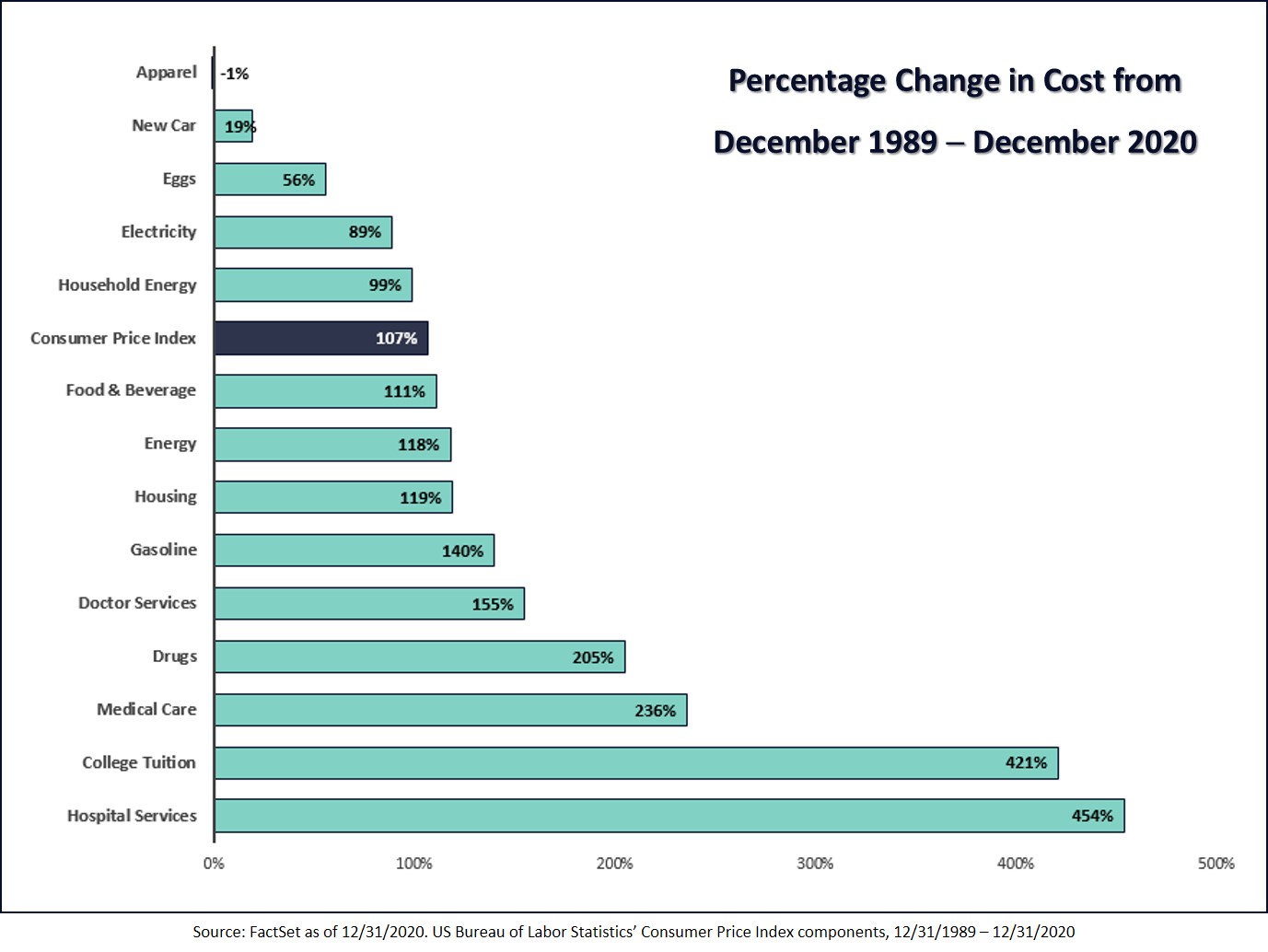
The article shares that “…the mean premium for family coverage increased by 55% from 2010 to 2020 (from $13,770 to $21,342) and employee contributions increased by 40% (from $3,997 to $5,588). Deductibles per enrolled individual increased 110% (from $646 to $1,364) and, to reduce monthly premium deductions from their paychecks, 31% of employees are now enrolled in high-deductible health plans.
“Partly as a result of employer-paid costs of employee benefits rising faster than employer income…take-home pay for most workers stagnated, with real median wages increasing 11% from $62,865 in 2007 to $69,560 in 2019, depriving employees of wage gains resulting from growth in their productivity.
“In the absence of intense counterpressure from insurers, hospitals and most other health care organizations have prioritized growth of high-priced services and developed costly marketing strategies, rather than restructuring to become a low-cost, high-quality solution for employees.”
The top three health insurers work aggressively to increase their monopoly market share of provider contracts that offer little value yet keep providers from pursuing arrangements with alternative payers. Compounding this, healthcare competition is severely hindered as more health systems, many of which don’t pay taxes, merge and purchase hospitals and physician practices, raising prices with each acquisition.
In examining insurance company revenue, profit, and shareholder dynamics, the authors illustrate, shockingly, that “Even if an insurer manages to improve profit margins by 20% while slowing per capita spending growth to 2%, their projected share prices would be lower than if per capita spending growth continued to increase at a 4% rate.” Read that again.
Employers and employees are effectively trapped in this dysfunctional industry matrix that prioritizes rapid growth and financial performance for shareholders.
Although higher healthcare costs are an obvious result of this aberrant system, other costs are more subtle and toxic. In an effort to maintain financial viability, employers often transfer higher health plan costs to employees through lower or no wage increases and higher payroll deductions, plans deductibles, co-insurance, and co-pays.
In the end, employees experience net wage stagnation, are unable to pay their out-of-pocket share when they use healthcare, avoid getting preventive and chronic care, and endure a diminishing quality of life as a direct result of an underperforming healthcare market.
What’s needed are seismic structural changes throughout the industry and better enforcement of regulations designed to accelerate price transparency and competition. In the meantime, employers play a key role in disrupting a system that actively works against the best interests of their organization and their employees.
How? By choosing a high-performance health plan that can save 30%+ over legacy insurance carrier plans while delivering high-quality care and improved member support. When better benefits are offered at a lower cost, employers can improve the quality of life of their workforce and their families.







 Vitori’s focus for the next few years will be growing its revenue and customer base and scaling its business nationwide. According to O’Brien, “We have found strong initial success, with client plan members in 48 states. And we’ve seen strong interest from brokers and advisors looking to save costs for their self-insured client health plans.”
Vitori’s focus for the next few years will be growing its revenue and customer base and scaling its business nationwide. According to O’Brien, “We have found strong initial success, with client plan members in 48 states. And we’ve seen strong interest from brokers and advisors looking to save costs for their self-insured client health plans.”